Review
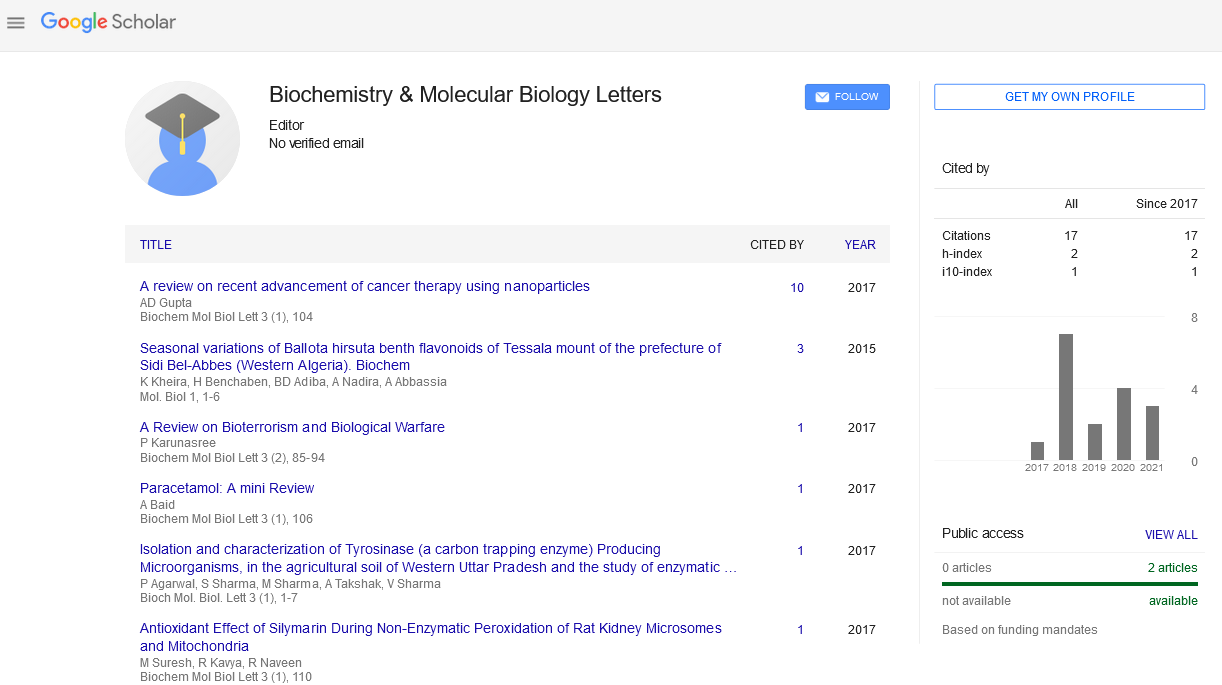
, Volume: 4( 1) DOI: 10.37532/2454-9304.2021.4(1).138Challenges with Mitochondrial Myopathies: Diagnosis Methods, Treatments and Ongoing Research
- *Correspondence:
- Patrick G. Pfeffer, Institute of Genetic Medicine, Newcastle University, Newcastle, United Kingdom; E-mail: p.g.pfeffer@ncl.ac.uk
Received: July 29, 2021; Accepted: August 12, 2021; Published: August 19, 2021
Citation: Pfeffer PG. Challenges with Mitochondrial Myopathies: Diagnosis Methods, Treatments and Ongoing Research. Biochem Mol Biol Lett. 4(1):138
Abstract
Introduction
Mitochondrial infections are brought about by abandons in mitochondria, which are energy processing plants found inside practically every one of the phones in the body. Mitochondrial infections that cause unmistakable solid issues are called mitochondrial myopathies (myomeans muscle and emotion implies sickness), while mitochondrial illnesses that causes both noticeable strong and neurological issues are called mitochondrial encephalomyopathies (encephalo alludes to the cerebrum). An average human cell depends on many mitochondria to meet its energy needs. The side effects of mitochondrial illness change, in light of the fact that an individual can have a special combination of sound and deficient mitochondria, with an extraordinary conveyance in the body. Much of the time, mitochondrial illness is a multisystem issue influencing more than one kind of cell, tissue, or organ [1]
Since muscle and nerve cells have particularly high energy needs, strong and neurological issues are normal provisions of mitochondrial illness. Other incessant confusions incorporate weakened vision, cardiovascular arrhythmia (strange heartbeat), diabetes, and hindered development. Typically, an individual with a mitochondrial illness has at least two of these conditions, some of which happen together so routinely that they are gathered into disorders.
Causes and symptoms of mitochondrial myopathies
Mitochondrial diseases are caused by genetic mutations. The genes involved in mitochondrial disease normally make proteins that work inside mitochondria. These proteins make up part of an assembly line that uses fuel molecules (sugars and fats) derived from food to manufacture ATP. The mitochondrion is the part of the body that makes ATP, the energy needed to make ATP. Some mitochondrial diseases are named for the respiratory chain that is affected by complex I deficiency. A cell filled with defective mitochondria becomes deprived of ATP and can accumulate toxic free radicals. The buildup of lactic acid in the blood is associated with muscle fatigue, and might damage muscle and nerve tissue. The ATP produced by mitochondria is the primary source of energy for muscle and nerve cells. Many muscular and neurological symptoms can result from the combined effects of energy deprivation and toxin accumulation in these cells [2].
The main symptoms of mitochondrial myopathy are muscle fatigue, weakness, and exercise intolerance. In some individuals, weakness is most prominent in muscles that control movements of the eyes and eyelids. The severity of any of these symptoms varies greatly from one person to the next, even in the same family. People with mitochondrial myopathies may experience muscle weakness in their arms and legs. People with the condition may also have difficulty swallowing and slurred speech. Some people might have trouble only with athletic activities like jogging or walking to the mailbox. Others may experience problems with everyday activities such as lifting a milk carton. Myoglobinuria can cause muscle cramps and pain after exercise. Cramps or myoglobinuria usually occur when someone with exercise intolerance "overdoes it" Moderate exercise appears to help people with mitochondrial myopathy maintain strength, doctors say. The protein myoglobin is released from the muscles into the urine (myoglobinuria) [3].
Tests for diagnosis
For patients with suspected mitochondrial myopathies (MM), demonstrative tests fall into two general classifications. The primary class of testing affirms the presence of brokenness in different organ frameworks and doesn't as such affirm a determination of MM. These tests are regardless essential to characterize the degree of the aggregate, to prohibit different problems, and to increment or abatement the clinical doubt of a MM finding. The tests chose are directed by the example of organ association in every individual patient. A portion of these tests merit extraordinary notice, in light of their capability to change patient administration. Heart examinations are of specific significance on the grounds that cardiovascular conduction imperfections can be lethal if not distinguished and are treatable with cardiovascular pacemakers. Endocrine examinations might distinguish diabetes mellitus, hypothyroidism, or development chemical inadequacy, which are all treatable. Patients with hearing or visual indications ought to be examined to get fitting guides whenever required. Dysphagia is normal in some mitochondrial conditions and can be dealt with dietary adjustment [4].
Normally, the specialist will arrange lab tests to search for diabetes and liver and kidney issues. The specialist is probably going to arrange an electrocardiogram (EKG) to check the heart for indications of arrhythmia and cardiomyopathy.
Treatments
There is presently no disease-modifying treatment available for MM. A variety of treatments (mainly nutritional supplements) have been studied in double-blind, placebo-controlled trials. Carnitine, creatine, CoQ10, cysteine, dichloroacetate, dimethylglycine, and creatine, CoQ10, and lipoic acid are among them. Efficacy in clinical disease endpoints has yet to be shown, despite the fact that multiple non-blinded trials and case reports have suggested efficacy. More research is needed to see if any of these drugs have therapeutic potential [5].
Future Research
The National Institute of Neurological Disorders and Stroke's (NINDS) objective is to seek fundamental information about the brain and nervous system in order to minimize the burden of neurological disease. The NINDS is part of the National Institutes of Health (NIH), the world's largest funder of biomedical research. Many of the genetic abnormalities that cause mitochondrial illnesses have been found by scientists. They've taken that knowledge and used it to develop animal models of mitochondrial disease that can be used to test potential treatments. Scientists have also developed genetic tests that enable for the reliable detection of mitochondrial abnormalities and provide useful data for family planning Most significantly, understanding the genetic abnormalities that cause mitochondrial illness brings up the prospect of designing tailored treatments. MNGIE is a unique example of how understanding mitochondrial disease genetics has led to a potential therapeutic. Genetic abnormalities in an enzyme called thymidine phosphorylase cause this condition (TP). The body accumulates metabolites termed nucleosides when the TP enzyme is lost. Some of these are DNA's building blocks, and their buildup appears to make mtDNA unstable. Researchers have demonstrated that giving people with MNGIE an infusion of blood-forming stem cells from a donor can repair the enzyme and lower nucleoside levels in the blood. Scientists hope to develop new approaches to treating mitochondrial diseases. People affected by mitochondrial disease often have a mixture of healthy and mutant mitochondria in their cells. Scientists hope to stimulate the birth of new mitochondria, encouraging the healthy ones to multiply and outnumber the mutants [6].
Finally, scientists have devised a method to prevent mutated mitochondria from passing from mother to child. The method would entail transferring nDNA from a woman with mtDNA illness into an egg cell from another woman with healthy mitochondria but no nDNA. The egg cell might then be fertilised and implanted into the woman who provided the nDNA using regular assisted reproduction techniques. Researchers tried the method in monkeys and found that it can create healthy nDNA donor children with no traces of the donor's mtDNA [7].
References
- DiMauro S, Bonilla E, Zeviani M, et al. Mitochondrial myopathies. Ann Neurol. 1985; 17(6):521-38.
- Schapira AH, Cock HR. Mitochondrial myopathies and encephalomyopathies. Eur J Clin Invest. 1999; 29(10):886- 98.
- de Barcelos IP, Emmanuele V, Hirano M. Advances in Primary Mitochondrial Myopathies (PMM). Curr Opin Neurol. 2019;32(5):715.
- Pfeffer G, Chinnery PF. Diagnosis and treatment of mitochondrial myopathies. Ann Med. 2013; 45(1):4-16.
- Milone M, Wong LJ. Diagnosis of mitochondrial myopathies. Mol Genet Metab. 2013; 110(1-2):35-41.
- Tarnopolsky MA, Raha S. Mitochondrial myopathies: diagnosis, exercise intolerance, and treatment options. Med Sci Sports Exerc. 2005;37(12):2086-93.
- Sharp LJ, Haller RG. Metabolic and mitochondrial myopathies. Neurol Clin. 2014;32(3):777-99.